Active Suicidal Ideation vs. Passive Suicidal Ideation
Suicidal ideation (thoughts of suicide) can feel like a very big topic, and it may not have been something your family or community discussed. Suicide and suicidal ideation have carried stigma for a long time. A significant part of this stigma was due to the criminalization of suicide in many places. If someone was “found guilty” of making a suicide attempt or “committing” suicide, the consequences (depending on the place and time) could have involved fines, jail time, confiscation of property, disrespectful burials, or prohibition of a funeral. Suicide has been decriminalized, which is an important reason to shift your language from “committed suicide” to “died by suicide.”
This blog will help break down the components of suicidal ideation and the difference between active and passive suicidal ideation.
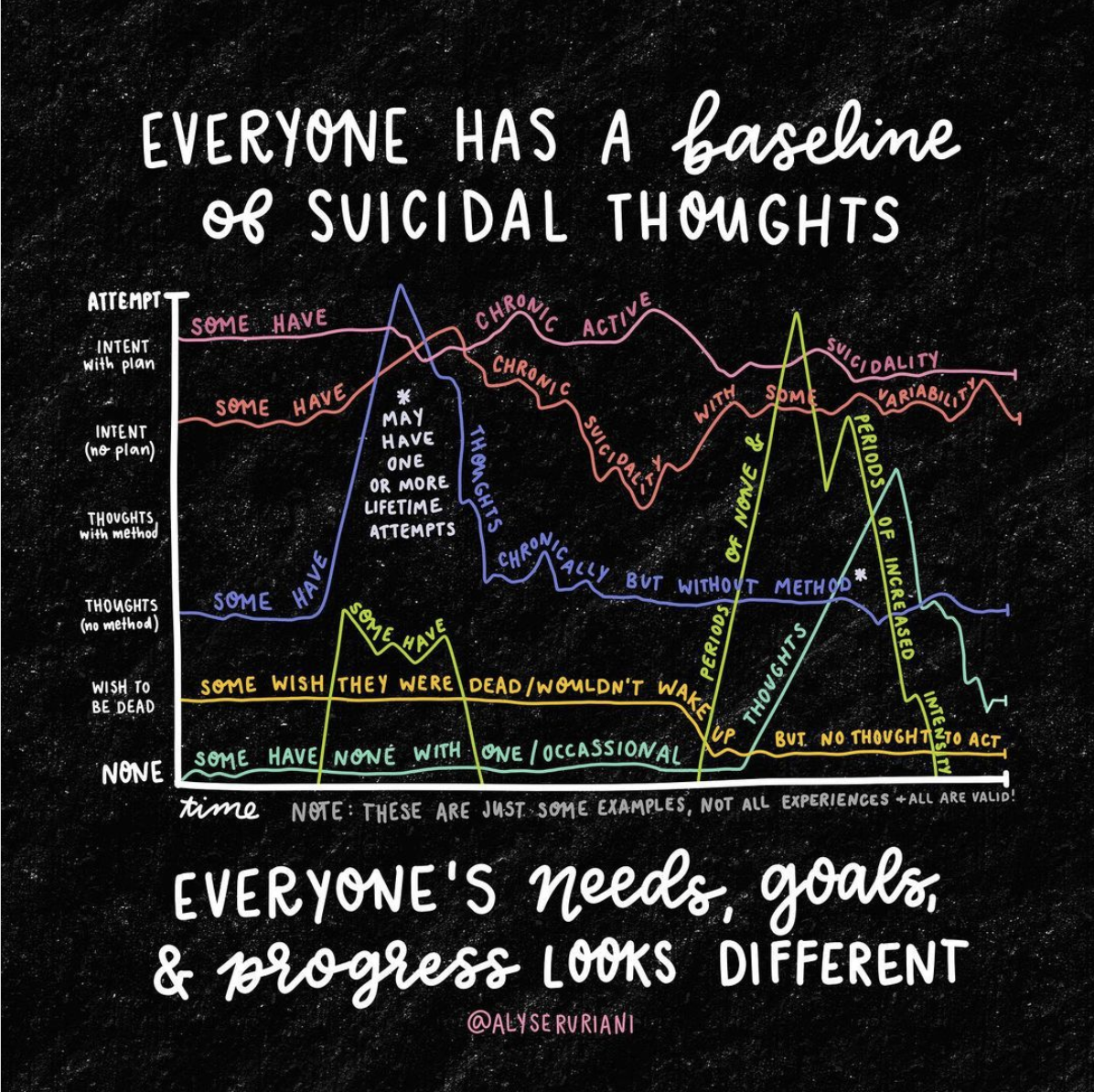
There are several different components of suicidal ideation.
Suicidal Ideation components
Thoughts: Are you having thoughts about suicide? Are you having thoughts of not wanting to be alive?
Plan: Do you have a plan of how you would kill yourself?
Means: What would you use to kill yourself? Do you have access
Intent: Are you thinking about following through with your plan?
Time Frame: Do you have a time frame of when you are thinking about following through with your plan?
Severity: How intense or severe are these thoughts?
If you aren’t used to having conversations about suicide, these questions might feel abrasive or overly direct. It makes sense that you may feel a little uncomfortable with these questions at first, but it is helpful to be direct when talking about suicide. Using direct language when talking about suicide communicates to the other person that you are not afraid of their suicidal ideation and that you are showing up to support them. Breaking down suicidal ideation into the components listed above also helps provide support and specific coping skills. Your therapist will assess these different components so that they know how to support you and use an appropriate intervention level. Hopefully, your therapist’s goal is to respond to your active SI with the least invasive intervention possible.
Active Suicidal Ideation
If someone is experiencing active suicidal ideation, they are more likely to have answers for the questions about these various components. Active SI means that, in some sense, you are having active thoughts about suicide. This might mean that you are thinking about how you would kill yourself (plan) but don’t have a time frame or intent. Maybe you have a plan of how you would kill yourself and access to means, but the severity is low. There is any number of combinations for the SI factors that you’re experiencing.
Someone with imminent risk for suicide typically has a plan, access to the means to follow through with their plan, a time frame, and the intent to follow through. This is a severe experience of SI. This severity level might require a more involved intervention to protect your safety. Interventions appropriate for imminent risk for suicide might involve friends and family in safety planning, considering an intensive outpatient program, or psychiatric hospitalization.
Passive Suicidal Ideation
Passive suicidal ideation is suicidal ideation without a plan. If you asked the questions above, you might get a response like, “I’m not sure; I just wish that I were dead.”
Some additional ways that passive suicidal ideation may be communicated are:
I wish I had never been born.
I would be okay if I didn’t wake up tomorrow.
Everyone is worse off with me in their lives.
Sometimes when I’m driving, I hope there’s an accident, and I don’t survive.
Passive SI does not include active thoughts about suicide, but it is still important to identify and take it seriously. It frequently comes from a place of dealing with anxiety and depression or feeling hopeless about a situation or symptoms. People who are experiencing passive suicidal ideation also need support and care. Dismissing someone’s passive SI is very reductive and will most likely lead to them feeling more alone.
If you are worried that someone you care about might be suicidal, ask them. The best way to support someone who is dealing with suicidal ideation is to have an honest conversation about it. This is the best starting place to identify what’s going on, what coping skills might help, and what support they need.
If you or someone you care about is experiencing suicidal ideation and needs therapeutic support, sign up for a free 30-minute consultation with our therapist matchmaker to find the therapist who’s your best therapeutic match.
All therapists at Woven Together Trauma Therapy are trauma-informed and specialize in treating all forms of trauma. We also offer EMDR Therapy, Ketamine Assisted Psychotherapy, and Brainspotting Therapy which have shown to be extremely effective in treating and healing treatment-resistant depression as well as helping with suicidal ideation. Want to read more about our unique therapy options?
These blogs talk more about the basics of EMDR Therapy:
You can read more about Ketamine Assisted Psychotherapy here:
If you would like to learn more about Brainspotting Therapy, check out our blog: What is Brainspotting?
Learn More About Our Approach To Therapy
For many survivors of complex trauma, the holiday season can be an evocative time. It can bring up anxiety about setting boundaries with difficult family members, grief regarding the people you are not spending the holidays with, or a sense of gratitude about the past year of growth and healing. Let’s talk about how to navigate the holiday season with complex trauma
In a sequel to the blog titled “How to Survive the Holidays with Your Partner,” I present to you some reflective questions and tips for how to cope with seeing family this holiday season!
You’ve done a whole lot of preparation: you’ve thought of what you want to tell your loved one, why, which triggers might come up and how to soothe yourself accordingly, which questions you’ll field (and won’t), when to take breaks, and whether you want to talk about the impact of your trauma on your relationship with the person you’re telling. You’ve even practiced soothing with triggers and taking breaks as needed to help your central nervous system feel safe when you’re distressed. The question is, how do we translate all of that work into having the conversation itself? Let’s talk about it.
There are many things that can lead to you no longer feeling connected to your partner or your relationship not functioning in the way you would like. Let’s dive into some key patterns that will kill the connection in your relationship.
Grief is a natural response to loss. It’s what our brains and our bodies do in reaction to the heartbreaking and devastating reality of loss. We humans are extremely resilient, and a vast majority of us will find a way back to living a meaningful life in our own time. Sometimes though, we can get derailed in that natural grieving process and that’s when it may be time to reach out for support.
So, you have an idea of what you want to say to a loved one about what you’ve gone through. You’ve thought about what might come up for you, and practiced soothing yourself in different ways. So what’s next? Planning for what you might specifically need from the conversation and person you’ll be telling. Let's talk about it.
I have had many patients come to therapy with me and say that talk therapy has not been helpful for them. Specifically, I hear the same complaint over and over: I felt like all I did was talk and open up, and I didn’t feel like there was a direction to therapy. When I hear complaints like this, I always want to start with some education about what trauma therapy looks like. Let's dive in.
Oomph, so you lost something. You lost something or someone that you loved. We often go so fast as a society, we celebrate the successes and wins, and we tend to ignore the pain associated with loss and grief, or put a time limit on it. Especially non-death-related grief and loss. This is an awful reality to endure for someone grieving. Let’s dive into how processing grief may look as a trauma survivor.
So, you’ve accepted that you get triggered pretty regularly because of What Happened, which is huge. It took so long to stop feeling like you were just “acting out for no reason,” and even if you still suspect you’re milking this whole trauma timeline, you also know you deserve a little bit more peace. In this blog post series, we’ll be covering how to have as safe and as containing of a conversation as possible with your loved ones about your trauma.
If you often find yourself in conflict with your partner which leads to yelling, there are a few things you can try to help create an environment for more productive conversation can occur. There should be very few reasons for you to yell or be yelled at, so trying a timeout protocol may help limit this way of engaging in conflict.
For many people with PTSD and trauma-related disorders, “dissociation” is a term that can seem scary and stigmatized. It can be important to demystify and educate ourselves on dissociation to better understand and validate our experiences.
What is shame? The dictionary definition is “a painful emotion caused by consciousness of guilt, shortcoming or impropriety.” One study even defined shame as “negative emotions in which the feeling of global self-evisceration is experienced.” Global self-evisceration. Oof! Shame is extremely unpleasant and painful, and it can affect one’s identity and self-esteem.
Many people are familiar with the idea of intersectionality, or how different aspects of our identities intersect with one another to make us who we are as people. What are the different ways that racial trauma shows up in our lives? Let’s dive in.
Psilocybin, the active ingredient in psychedelic mushrooms, is probably going to be legalized for therapeutic use in the United States in the next two years, and that’s on trauma treatment progress. Let’s dive into part III in what that may look like for trauma treatment.
There are five stages in the family life cycle and the stage of parenting is considered the most stressful. This is the time in which divorce rates are at their highest, sex is at its lowest and couples feel the most disconnected. Here are some ideas to help maintain your relationship during this hectic time.
We might be only a year or two away from legalizing psilocybin, the active ingredient in psychedelic mushrooms, for therapeutic use in the United States. Let’s talk about what that might look like for future trauma treatment.
With the well-earned buzz around this evidence-based approach to healing trauma, there are also plenty of misunderstandings. Let’s take a look at some common myths so that you are prepared to advocate for yourself and make decisions about your mental healthcare.
Microaggressive trauma describes the excessive and continuous exposure to subtle interpersonal and systemic discrimination that lead to trauma symptoms like sensitivity to threat, anxiety, and hyperarousal.
When I ask myself: “What do all human beings have in common?” I always come to the same conclusion: we all have a wounded child that lives within us. That child may have been wounded by different systems and in different ways, but in the end, even if our identities are filled with privilege, we all have been injured, in one way or another in our early relational dynamics and that is part of being human.
What is a situationship, you ask? A situationship “is often discussed as being similar to a friends-with-benefits relationship, which usually involves sexual activity without a commitment to be exclusive to each other. The definition further explains that “a situationship is often described as a relationship that is more than friendship but less than a committed relationship.” So what are we to do if we find ourselves in one of these? Below are some ideas!
We’re in our shrooms era. That’s right. I said it. Psilocybin is having a glow-up in the psychotherapeutic community, and we are excited about what that means for future trauma treatments.
I can’t tell you how many times I’ve heard, “I felt like my White therapist just didn’t get it” or “I quit therapy when my therapist told me to just set boundaries with my immigrant parents.” Don’t get me wrong, I think any therapist of any race can be culturally inclusive with the right training, consideration, and sensitivity. For example, I trust the diverse team here at Woven to be thoughtful of issues of (de)colonization, Asian American frame switching, and being flexible with interventions to consider unique aspects of identity.
Throughout my practice as a somatic trauma therapist, I see patients whose painful experiences muted their connection to the body. For trauma survivors, focusing on their body sensations - even if only for a brief second - can become extremely overwhelming because it brings them back to their experiences of being neglected, abandoned, or abused. Let’s explore the concept of somatic awareness and to help trauma survivors understand why this practice holds the key to understanding emotions, traumas, and overall well-being.
You may be feeling vulnerable, hopeful, anxious, excited, uncertain, fearful, or any combination of emotions as you await your first session. Questions like what to expect during a 90-minute intake, what does a regular 45-minute session look/feel like, or how to plan/prepare for therapy in general may be on your mind (or search history). This is completely normal! Megan Bakva, ASW talks about her approach to trauma therapy.
Some may assume that grooming only happens to children or adolescents, but grooming happens to adults as well. Quite surprisingly, sexual abuse occurs by someone the victim knows 93% of the time. This might include a family member, friend, neighbor, teacher, coach, youth leader, supervisor, etc. Learn more about the common grooming tactics and impacts of grooming here.
How does racism show up in our body, thoughts, and emotions? People who are familiar with racism may know that it is acknowledged as a public health crisis by the American Public Health Association. But how do daily experiences of racism, discrimination, and microaggressions affect us psychologically and in our trauma symptoms? How does it show up in our bodies, thoughts, and emotions? Let’s dive in.
Have you ever found yourself scrolling on your phone for hours and then not being able to remember what you watched? Or maybe you feel overwhelmed all the time. Or numb. Does this sound familiar? Let’s talk about the freeze response and dissociation 101.
If this time of the year brings up anxiety, depression, hopelessness, or loneliness for you, your body can be at the center of it. For many people, the memories that arise are filled with joy and happiness, for others - survivors of childhood trauma - the body remembers this season with complex emotions.
There are a lot of things happening during the holiday season. Because the holidays are usually very nostalgic for people, it’s almost like our brains are primed to remember all our childhood trauma. So how can we survive the holidays with our romantic relationship intact? JHere are some ideas that might help.
Calendar filling up with events? Booking those tickets back to your hometown? A familiar sense of anxiety creeping in? You’re not alone. As the lights and holiday spirit go up around town, many of us are faced with less-than-festive feelings.