Getting Ready To Get Things Done After Trauma
You know most people think of productivity as doing the most at the flip of a switch. You also know that doesn’t describe you outside of the rare day you finish some things, but also go into that fuzzy space where fingernails magically get chewed off and you forget to feed yourself, let alone blink. And you know productivity should be attainable. It should account for people like you with PTSD. We talked about why it was so hard to be productive in my last blog. Now let’s talk about how to start getting things done.
The good news? It’s not only possible to be productive with PTSD, but in a way that helps manage your symptoms.
Let’s review how those PTSD symptoms can contribute to the dust on your to-do list*
You keep randomly getting triggered and pulled out of whatever you’re doing
You can’t focus to save your life
You can’t remember what you were supposed to be focusing on in the first place
You avoid things (so many things, including that to-do list)
Each time that list grows, you want to chew your nails clear off all over again
You blame all of this on how “lazy” you are
Once you see how PTSD has been sneaking up on you, it might seem like doing almost anything can make everything worse.
That’s why, for this part of my productivity post-trauma series, I’m going to focus on getting to the point where you can start a task, and complete it with less distress and shame.
Problem #1: You keep getting triggered.
This might look like suddenly thinking about traumatic memories, having flashbacks, feeling numb, or getting the urge to walk, run, hide, or fight something. And boy, does it make it hard to just sit down and do anything.
Tip #1: Try and figure out what’s triggering you.
When are you getting triggered? Where are you getting triggered? What happened right before you started feeling off? Were you thinking about a certain task? Did you see something? Smell something? Feel something?
You might really want a quick productivity hack, but when you have PTSD, it helps to take a step back first and find the patterns in how your brain is coping with your day-to-day. The more you know your triggers, the less likely it is that you’ll stumble into one without warning and get yanked out of the present when you want to be doing something. The goal here isn’t to avoid your triggers–that can be helpful in a pinch, but avoiding reminders of your trauma is also a symptom of PTSD (and ultimately, with effective treatment, you’ll get triggered less and less anyway). The goal is to figure out when a trigger might happen ahead of time so that you can know when and how (we’re getting there) to help your nervous system stay a little calmer.
A lot of people know their Big Triggers, but to find ones that you might not know about already, track your symptoms throughout the day. Track when you’re:
Stuck in a flashback of your trauma
Wanting to walk, run, hide, or fight something (or someone)
Thinking about the trauma in general
Feeling (particularly) bad
Feeling anxious or really on edge
Forgetting what you just did, or parts of it
Distracting yourself (with that tried and true show you need to binge to forget the world, or your phone…or that edible that’s not going to eat itself tonight)
Next to any of those instances, write down what happened beforehand (i.e., what you were doing, where you were doing it). Try it for a couple of days until you notice patterns. Any triggers you can identify will be a huge help (both in getting things done and treatment–hello therapy, tracking how you feel when, and coming in with that much more understanding of where you’re at!). This leads me to the next tip.
Tip #2: Keep an eye out for sneaky triggers.
Do you know how many times people have told me they don’t get triggers anymore, only to then describe hours they lost track of at their desk, scrolling through (painful) social media, and getting more and more furious with themself after getting a text from their mom? Or thinking about how they have to call a doctor for a follow-up appointment (let alone their health insurance)? Or feel like the moment they stop going and going and going, they’ll be in danger, but they stopped “going” and lost focus all the same?
Triggers don’t have to be full-blown flashbacks where your trauma flashes before your eyes. They can be overwhelm in response to anything that reminds you of:
A childhood that was chockfull of trauma (no matter how minor you think it was)
Issues you’re nervous about that someone in a position of authority over your mind or body didn’t handle with care
Worries about being stuck with your thoughts because: being still feels like being frozen, which feels like how you felt whenever your trauma happened
And a thousand other things!
That includes feeling trapped, stuck, or powerless for a lot of people.
Add those types of trauma responses to the list you started!
One of the toughest things about trauma is that it makes it a lot harder to sit with yourself and connect with what’s happening. Which means that noticing what’s happening inside and writing it down can be frustrating and draining, not to mention another source of shame and self-blame.
And that leads me to problem #2: You can’t figure out how you’re feeling.
You might be able to explain your existential dread as easily as how to go through the drive-through at McDonald’s (the inevitable doom of the world as we know it could be described through today’s headlines on Reddit alone, amirite?). But if I were to ask you what you feel in your body (e.g., Are you sad? Angry? Numb? In your chest, arms, neck, back, or somewhere else? What does it feel like in that specific place?), what would you say?
If it’d be hard to answer, you’re not alone.
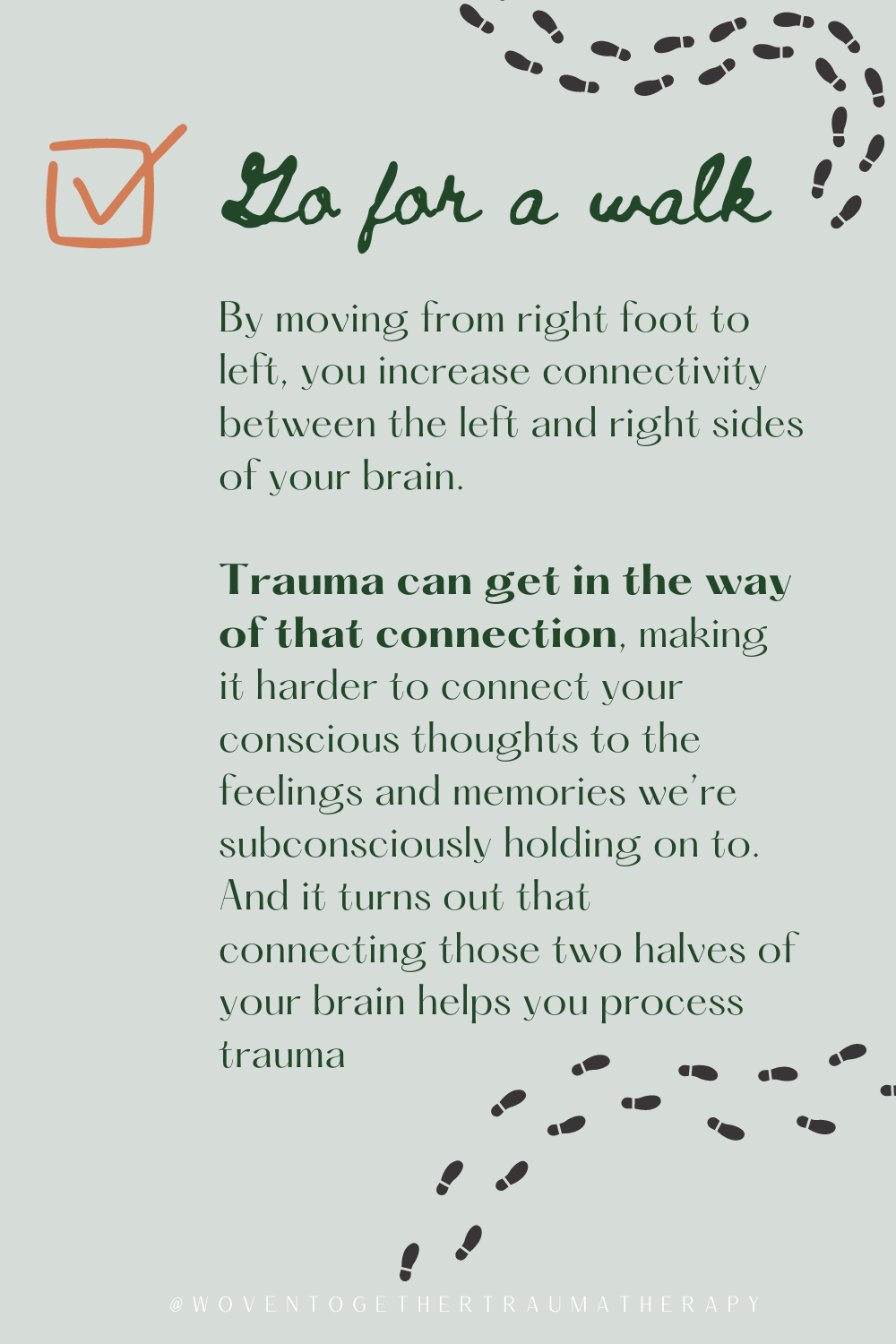
Tip #1: Take a walk.
Of course, you might be thinking. She’s just saying what everyone says. As if that’s helped me.
I gotchu. I’m not assuming you’re the last person on earth who hasn’t heard of walking.
When it comes to trauma recovery, the big benefits of walking I want to emphasize are twofold:
By moving from right foot to left, you increase connectivity between the left and right sides of your brain. Trauma can get in the way of that connection, making it harder to connect your conscious thoughts to the feelings and memories we’re subconsciously holding on to. And it turns out that connecting those two halves of your brain helps you process trauma** Tl;dr: walking, no matter how slow, is a way to help you figure out what’s going on inside you.
You can use it as a chance to reorient. It’s hard to focus when you’re scanning your environment for threats to your safety 24/7. So if you consciously use a walk as a time to focus on things you enjoy looking at, it can retrain your brain over time to come out of danger scan-mode and connect with your body.*** Meaning you’ll be better able to figure out how you feel beyond “AAAAHHHH OVERWHELMED DKJHKAJSDKAS!”
Tip #2: sit somewhere with a good view and tap on your chest.
What?! I know. Hear me out; it’s not just a California heart-location thing.
If you cross your arms over your chest and take a couple minutes to alternate tapping your left hand on your right side, followed by your right hand on your left side, it’ll encourage that same connectivity between the left and right sides of your brain. And you can still look for things in front of you that you like looking at. Left brain/right brain connectivity and reorientation accomplished.
Now, let’s say you’ve tried walking and tapping and it just ain’t doing it for you. I have another activity to help you feel into where you’re at and why.
Tip #3: Breathe
We hear this life hack (more like life-must imho) a lot, so it sounds like a one-size-fits-all approach. But when you panic (which you subconsciously tend to do if you feel like tons of things around you are life-or-death threats), taking deep breaths where your exhales are longer than your inhales can bring you out of the panic. Just observe if anything changes in your body and mind as you breathe.
See if your shoulders relax. Or your thoughts stop racing. Or you feel less bad and more neutral.
If you notice any of those things, guess what? You’re more in touch with your body and mind.
These three activities may sound simple, but they’re not. They take practice, and doing them when with post-traumatic stress makes it way harder.*** But the goal is to get you to a place where you can figure out what’s triggering you and how you feel, and as you figure out what’s triggering you, these things can get you there. One step, tap, or breath at a time.
In the final blog post in my series on productivity post-trauma, we’ll talk about how to actually do the things. Spoiler alert: I won’t be giving you the key for how to do 101 things in 8 hours–I prefer not making you feel like your brain is on fire, thank you very much.
Until then, discover which triggers might be coming out of left field for you and practice checking in with how you feel. Those are serious symptom management goals you can add to and check off your new-and-improved list when we get to it next time. ✅
Did this ring true for you? Looking for a therapist who specializes in Complex PTSD and procrastination? Our therapists and coaches can help. Book a therapy or coaching appointment with our therapist matchmaker to begin your healing journey today. (Therapy is only available in CA.)
Interested in learning more about our unique approach to trauma therapy?
These blogs talk more about the basics of EMDR:
You can read more about Ketamine Assisted Psychotherapy here:
References:
*Chen, J. J. (2019, April 10). Productivity Hacks Don’t Work When You Have Mental Illness. Elemental. https://elemental.medium.com/productivity-hacks-dont-work-when-you-have-mental-illness-4635239860c6
**Bilateral Stimulation: What It Is, Effects, & Use in EMDR. (2022, October 24). Choosing Therapy. https://www.choosingtherapy.com/bilateral-stimulation/
***Kearney, B. E., & Lanius, R. A. (2022). The brain-body disconnect: A somatic sensory basis for trauma-related disorders. Frontiers in Neuroscience, 16.https://www.frontiersin.org/articles/10.3389/fnins.2022.1015749